Cultural competency in healthcare is crucial for improving patient outcomes and satisfaction, especially in diverse communities like Longmont. It helps providers understand and respect different cultural backgrounds, facilitating effective treatment of issues like PTSD and anxiety. In Longmont, addressing biases through self-reflection, education, and training—including conflict resolution techniques—is vital for delivering equitable care. Robust communication strategies tailored to cultural nuances enhance patient engagement and care quality. The Longmont Post-Traumatic Stress Disorder (PTSD) Therapy program serves as a model for culturally sensitive care, bridging mental health disparities and promoting holistic mental wellness through specialized therapy, coaching, and stress management techniques.
Healthcare provider cultural competency training is an essential component of modern medical practice, addressing the critical need for empathetic and effective care in a diverse society. This article explores key aspects of cultural competency, focusing on why it matters, identifying and overcoming biases, and effective communication strategies for diverse patients. We also delve into a case study of Longmont Post-Traumatic Stress Disorder Therapy, showcasing a model program that prioritizes cultural sensitivity.
- Understanding Cultural Competency in Healthcare: Why It Matters
- Identifying and Overcoming Biases in Clinical Settings
- Effective Communication Strategies for Diverse Patients
- Case Studies: Longmont Post-Traumatic Stress Disorder Therapy as a Model
Understanding Cultural Competency in Healthcare: Why It Matters

Cultural competency in healthcare is more than just a buzzword; it’s an essential aspect that significantly impacts patient outcomes and overall care satisfaction. It refers to the ability of healthcare providers to understand, appreciate, and respect diverse cultural backgrounds, beliefs, and values, especially when treating patients from different ethnic, racial, or social groups. Given the increasing diversity in communities across the globe, including cities like Longmont with its vibrant tapestry of cultures, this skill set is crucial.
When healthcare providers are culturally competent, they can better address complex issues such as post-traumatic stress disorder (PTSD) and anxiety among patients from various cultural walks of life. For instance, a study on PTSD treatment in urban areas might reveal unique challenges faced by diverse communities, requiring tailored interventions and communication strategies to ensure effective anxiety relief and stress reduction methods. Moreover, this competency fosters open dialogue, ensuring patients feel heard and understood, which is vital for building trust and promoting mental wellness. The integration of cultural sensitivity into healthcare delivery can lead to improved patient adherence to treatment plans and better overall mental wellness podcast series production.
Identifying and Overcoming Biases in Clinical Settings

In clinical settings, biases—conscious or unconscious—can significantly impact patient care and outcomes. Healthcare providers, despite their best intentions, may hold preconceived notions or stereotypes that affect their interactions with diverse patient populations. For instance, a study might reveal a bias in diagnosis or treatment among patients with Post-Traumatic Stress Disorder (PTSD), stemming from cultural misunderstandings or personal prejudices. In Longmont, Colorado, where a diverse community coexists, addressing these biases is paramount to delivering equitable healthcare.
Identifying and overcoming biases requires ongoing self-reflection and education. Burnout Prevention Strategies for Healthcare Providers often emphasize the importance of cultural competency training, which includes Conflict Resolution Techniques and Self-Esteem Improvement exercises. By fostering an environment where providers actively question their assumptions and learn from patients’ unique experiences, institutions can enhance patient satisfaction and clinical outcomes. This proactive approach not only benefits individual patients but also contributes to a more inclusive healthcare system that respects and values every patient’s journey.
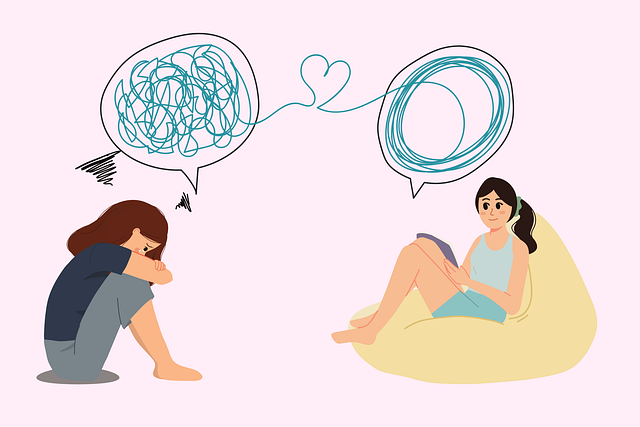
Effective Communication Strategies for Diverse Patients

Effective communication between healthcare providers and diverse patients is a cornerstone of quality care. It involves understanding and adapting to cultural differences in language, non-verbal cues, and personal space. For instance, a patient from a community with strong familial bonds may prefer involving their family in decision-making processes, while another patient struggling with Longmont Post-Traumatic Stress Disorder (PTSD) might require a more sensitive and tailored approach.
Training in cultural competency equips providers to employ strategies that facilitate meaningful communication. This includes learning about different emotional healing processes, coping skills development, and stress reduction methods relevant to diverse populations. By doing so, healthcare professionals can create an environment where patients feel heard, respected, and empowered to participate actively in their treatment plans, ultimately enhancing the effectiveness of care delivery.
Case Studies: Longmont Post-Traumatic Stress Disorder Therapy as a Model

The Longmont Post-Traumatic Stress Disorder (PTSD) Therapy program serves as a compelling model for healthcare provider cultural competency training, particularly in addressing mental health disparities. This initiative focuses on providing specialized therapy to individuals from diverse backgrounds who have experienced trauma, often overlooked in mainstream mental health services. By incorporating culturally sensitive approaches, the program ensures that participants receive tailored care that respects their unique experiences and perspectives.
Incorporating case studies like Longmont PTSD Therapy highlights the importance of Mental Health Policy Analysis and Advocacy in shaping inclusive practices. The development of Mental Wellness Coaching Programs can further enhance these efforts by offering ongoing support and education to healthcare providers. Additionally, focusing on Stress Management techniques within this context empowers individuals to cope with trauma-related symptoms, fostering a holistic approach to mental wellness.
Cultural competency training is an indispensable tool for healthcare providers, ensuring they can offer effective and equitable care to a diverse range of patients. By understanding cultural nuances, identifying and addressing biases, and adopting effective communication strategies, professionals like those at the Longmont Post-Traumatic Stress Disorder Therapy center can significantly improve patient outcomes. This article has explored these critical aspects, emphasizing the importance of continuous learning and adaptation in healthcare to meet the needs of all individuals.