Cultural competency in healthcare is vital for effective treatment of adults who have experienced child abuse (Therapy for Adults Child Abuse), addressing biases that can hinder progress. By integrating cultural sensitivity training into medical curricula, emphasizing active listening and open communication, healthcare providers can offer tailored support like mental wellness journaling to empower patients from diverse backgrounds to heal. This multifaceted approach improves patient outcomes, enhances trust, and fosters inclusive environments, ensuring justice in care for all individuals regardless of their cultural background.
In today’s diverse healthcare landscape, cultural competency is no longer an option—it’s a necessity. This comprehensive guide explores the critical role of cultural competency training for healthcare providers, focusing on its impact on effective treatment and addressing biases that may hinder progress in therapy for both adults and child abuse cases. We delve into actionable strategies to empower providers, ensuring equitable care for all patients.
- Understanding Cultural Competency in Healthcare: A Necessity for Effective Treatment
- The Impact of Cultural Biases on Adult and Child Abuse Cases
- Strategies for Training Healthcare Providers to Address Cultural Inequalities in Therapy
Understanding Cultural Competency in Healthcare: A Necessity for Effective Treatment

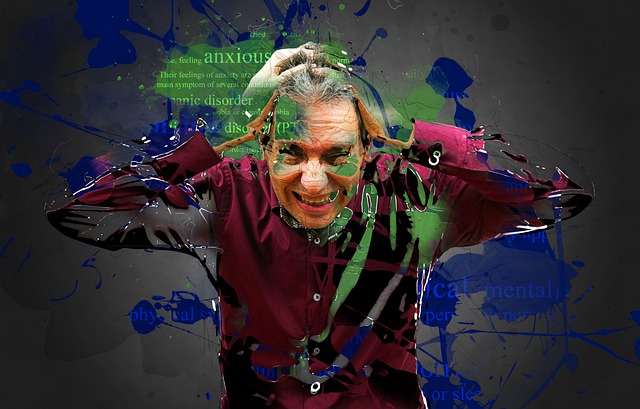
Cultural competency in healthcare is no longer a luxury; it’s an absolute necessity for providing effective treatment and promoting the emotional well-being of diverse patient populations. In a world where cultural differences can profoundly impact health outcomes, understanding and respecting these variations are key to delivering quality care. For instance, certain communities may have unique beliefs around health and illness, influencing their willingness to seek medical attention or adhere to treatment plans.
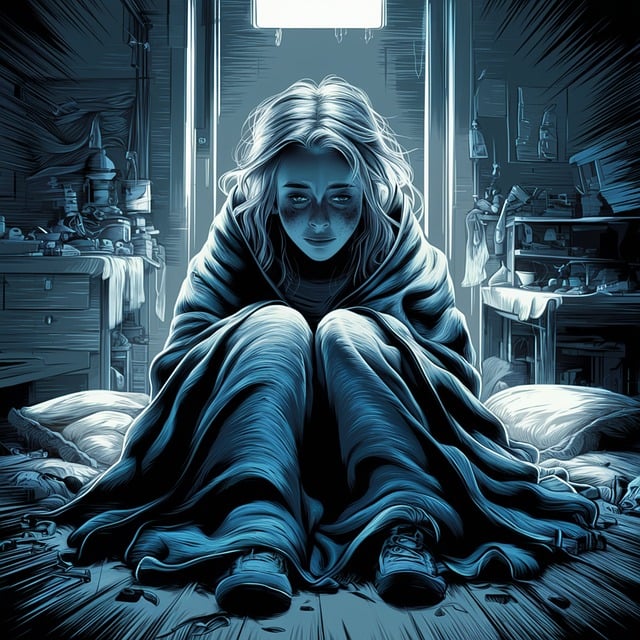
This is especially critical when addressing sensitive issues like therapy for adults who have experienced child abuse. Cultural competency allows healthcare providers to offer trauma support services tailored to the specific needs of these individuals, considering their cultural context. Techniques such as mental wellness journaling exercises can be integrated into care plans, but only if providers are attuned to cultural nuances and barriers. Ultimately, embracing cultural competency is about fostering inclusive environments that empower all patients to heal and thrive.
The Impact of Cultural Biases on Adult and Child Abuse Cases

Cultural biases can significantly impact the way abuse cases, particularly involving adults and children, are perceived and handled by healthcare providers. These biases, often unconscious, can lead to misjudgments and inadequate responses to sensitive situations. For instance, a provider’s assumptions about a patient’s behavior or motivation based on their cultural background might hinder effective therapy for adults who have experienced child abuse. Similarly, when dealing with child abuse cases, cultural differences in understanding of family dynamics and reporting behaviors can create challenges.
Understanding the role of cultural biases is crucial to ensuring justice and support for victims. Incorporating Mind Over Matter principles and Stress Reduction Methods into training curricula can help healthcare professionals enhance their Mental Health Awareness. By recognizing and addressing these biases, providers can offer more empathetic care, improve outcomes, and contribute to a more just system for all individuals, regardless of their cultural backgrounds.
Strategies for Training Healthcare Providers to Address Cultural Inequalities in Therapy

Training healthcare providers to address cultural inequalities in therapy requires a multifaceted approach. One key strategy involves incorporating cultural sensitivity in mental healthcare practice into the curriculum for all medical and therapeutic professionals. This includes teaching them to recognize and respect diverse cultural beliefs, values, and practices related to health and wellness, particularly when dealing with sensitive issues like therapy for adults and child abuse. Sensitivity training should also emphasize active listening, non-judgmental attitudes, and open communication to foster trust between providers and patients from different backgrounds.
Additionally, mental health education programs design should prioritize the development of a robust self-care routine development for better mental health among healthcare providers. This is crucial as burnout and stress can negatively impact their ability to deliver culturally competent care. By promoting healthy work-life balance and providing resources for stress management, mental health professionals can enhance their cultural sensitivity and improve patient outcomes, especially when addressing complex issues like abuse across various cultural contexts.
Cultural competency training is a game-changer in healthcare, especially when addressing issues like adult and child abuse. By recognizing and understanding the impact of cultural biases, healthcare providers can ensure more effective therapy and improved outcomes for diverse patient populations. Implementing comprehensive training strategies, such as those discussed in this article, can help bridge cultural inequalities in treatment, fostering a more inclusive and responsive healthcare system. This approach is vital to providing quality care and promoting healing across various cultural contexts, especially in cases of abuse.