In today's healthcare landscape, especially within Lakewood, cultural competency is key for effective OCD therapy. Understanding patients' diverse backgrounds, beliefs, and values fosters trust and improves communication, leading to better adherence to treatment plans. Unaddressed cultural differences in mental health care can widen disparities, particularly affecting marginalized communities. Lakewood Obsessive Compulsive Disorder (OCD) Therapy stands out with its culturally sensitive approach, integrating Mental Health Policy Analysis, Advocacy, and Emotional Intelligence. Effective training programs for healthcare providers should cultivate genuine cultural competency through interactive workshops and case studies. Continuous evaluation, feedback mechanisms, and self-reflection are vital to improve patient outcomes tailored to diverse communities' needs, including those seeking Lakewood Obsessive Compulsive Disorder Therapy.
Healthcare provider cultural competency training is an essential component of delivering effective and equitable patient care. In a diverse society, understanding cultural nuances can significantly impact treatment outcomes, especially in mental health practices like Lakewood Obsessive Compulsive Disorder Therapy (LOCDT). This article explores the necessity of cultural competency, its effects on patient results, and provides a case study highlighting successful culturally sensitive approaches. Additionally, it offers insights into designing training programs, continuous evaluation, and fostering long-term growth in this critical area.
- Understanding Cultural Competency in Healthcare: A Necessity for Effective Patient Care
- The Impact of Unaddressed Cultural Differences on Mental Health Treatment Outcomes
- Lakewood Obsessive Compulsive Disorder Therapy: A Case Study in Culturally Sensitive Practice
- Designing and Implementing Comprehensive Training Programs for Healthcare Providers
- Continuous Evaluation and Improvement: Ensuring Long-Term Cultural Competency Growth
Understanding Cultural Competency in Healthcare: A Necessity for Effective Patient Care

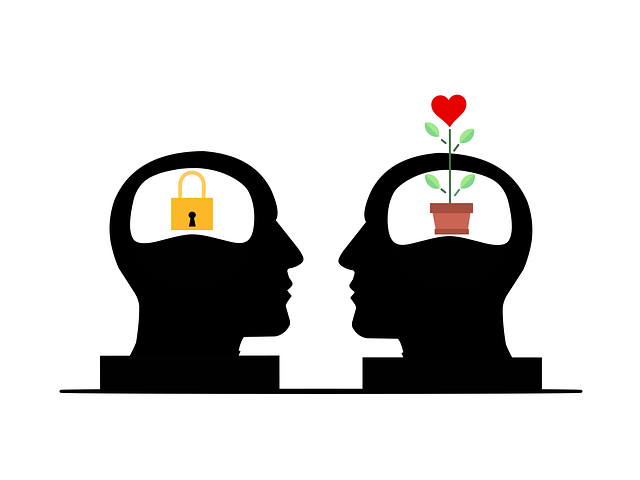
In today’s diverse healthcare landscape, cultural competency is no longer a nice-to-have but an essential requirement for effective patient care. Understanding and respecting different cultures, beliefs, and values are crucial aspects of providing quality medical services. This is especially relevant in areas like Lakewood, where patients may represent a wide range of ethnic, racial, and social backgrounds, including those seeking treatment for conditions such as obsessive-compulsive disorder (OCD). Healthcare providers who lack cultural competency risk misinterpreting patient needs, leading to suboptimal outcomes and potential harm.
Cultural competence involves developing inner strength, emotional intelligence, and empathy building strategies that enable healthcare professionals to navigate complex cultural nuances. By fostering these skills, medical staff can create a welcoming environment where patients feel heard, respected, and understood. This, in turn, enhances patient trust, improves communication, and promotes adherence to treatment plans. For instance, when dealing with Lakewood residents struggling with OCD or other mental health issues, culturally sensitive care can significantly impact the effectiveness of therapy and overall well-being.
The Impact of Unaddressed Cultural Differences on Mental Health Treatment Outcomes

Unaddressed cultural differences can significantly impact mental health treatment outcomes, especially for communities with unique or marginalized identities. When healthcare providers lack cultural sensitivity and competence, they may inadvertently perpetuate barriers to effective care. For instance, individuals from diverse ethnic and racial backgrounds often face challenges in accessing quality mental health services due to language barriers, differing therapeutic norms, and historical traumas. These factors can lead to misdiagnoses, inadequate treatment plans, and higher rates of treatment discontinuation.
In the context of Lakewood Obsessive Compulsive Disorder (OCD) Therapy, for example, a therapist lacking cultural competence might not recognize or appreciate the distinct ways OCD manifests across diverse populations. This oversight could result in ineffective treatments tailored to Western norms, potentially causing frustration and poor adherence among patients from non-dominant cultural groups. Integrating Cultural Sensitivity in Mental Healthcare Practice, along with robust Mental Health Policy Analysis and Advocacy, is crucial to ensuring equitable access to quality mental wellness coaching programs development, ultimately improving treatment outcomes for all individuals seeking support.
Lakewood Obsessive Compulsive Disorder Therapy: A Case Study in Culturally Sensitive Practice

Lakewood Obsessive Compulsive Disorder (OCD) Therapy serves as a compelling case study in culturally sensitive mental health practice. By understanding and respecting the unique cultural backgrounds and beliefs of their clients, therapists can create an environment that fosters trust and engagement. This is particularly crucial when addressing OCD, a condition that often intersects with various cultural and ethnic identities.
The therapy center’s approach involves integrating Mental Health Policy Analysis and Advocacy into their treatment plans, ensuring that interventions are not only effective but also culturally responsive. Therapists guide clients through Mental Wellness Journaling Exercise Guidance, helping them explore and express their experiences while considering the impact of cultural factors on their mental wellness. Emotional Intelligence plays a vital role in this process, allowing therapists to navigate complex interpersonal dynamics and provide care tailored to each individual’s needs.
Designing and Implementing Comprehensive Training Programs for Healthcare Providers

Designing comprehensive training programs for healthcare providers is a multifaceted process that requires careful consideration to address diverse learning needs and cultural contexts. These programs should go beyond surface-level awareness and aim to foster genuine cultural competency, enabling providers to connect with patients from various backgrounds on a deeper level. Incorporating interactive workshops, case studies reflecting real-life scenarios, and role-playing exercises can create engaging environments for knowledge retention.
At the core of these training initiatives, organizations like Lakewood Obsessive Compulsive Disorder Therapy (LACDT) offer valuable resources, emphasizing not only mental health awareness but also burnout prevention and self-esteem improvement. By integrating social skills training, healthcare professionals can enhance their ability to communicate effectively with patients from different cultures, reducing potential barriers and promoting inclusive care. Ultimately, these programs should seek to empower providers, ensuring they feel equipped to navigate complex cultural dynamics while delivering compassionate and personalized patient care.
Continuous Evaluation and Improvement: Ensuring Long-Term Cultural Competency Growth

Cultural competency is an ongoing journey rather than a one-time event. Healthcare providers must embrace continuous evaluation and improvement to ensure long-term growth in this critical area. Regularly assessing patient interactions, feedback mechanisms, and self-reflection can help identify cultural blind spots or areas of improvement. By implementing structured feedback loops, healthcare professionals can gather insights from diverse patient populations, colleagues, and community members, fostering an environment where learning and adaptation are valued.
This process involves active listening to patients’ unique experiences, perspectives, and needs, going beyond surface-level interactions. For instance, a therapist in Lakewood Obsessive Compulsive Disorder (OCD) therapy might utilize mindfulness meditation as an Empathy Building Strategy during sessions, encouraging both patients and practitioners to cultivate awareness of their thoughts, emotions, and behaviors without judgment. Over time, such practices can lead to enhanced cultural competency, better patient outcomes, and improved mental health services tailored to diverse communities’ needs, ultimately reducing anxiety relief barriers.
Healthcare provider cultural competency training is no longer a choice, but an indispensable tool for delivering effective patient care. As evidenced by the case study of Lakewood Obsessive Compulsive Disorder Therapy, culturally sensitive practices can significantly improve treatment outcomes. Implementing comprehensive training programs, continuously evaluating progress, and fostering a commitment to ongoing learning ensures that healthcare providers are equipped to navigate the complex landscape of cultural differences. By doing so, we not only enhance patient satisfaction but also contribute to more positive mental health outcomes for all individuals, regardless of their cultural background.