Dissociative Disorder (DD) is a complex mental health condition characterized by identity and sensory disruptions, often arising from traumatic events. Effective therapy involves risk assessment, integrating emotional intelligence, and personalized interventions focusing on emotion regulation and coping strategies. A Comprehensive Harm Minimization Plan, tailored through therapy, includes crisis management, stigma reduction, and depression prevention, ensuring long-term stability and improved quality of life for individuals with DD. Continuous monitoring and adjustment guided by evidence-based practices empower clients to navigate their conditions and make informed decisions about their well-being.
Risk assessment and harm minimization planning are crucial components in the therapy for Dissociative Disorder (DD), a complex mental health condition characterized by altered identity or memory. This article delves into the understanding of DD, focusing on symptoms and causes. It explores the role of risk assessment in effective treatment, presents strategies for harm minimization, and provides a step-by-step guide to creating a comprehensive plan. Additionally, it discusses implementing and monitoring the plan within a therapeutic framework.
- Understanding Dissociative Disorder: Symptoms and Causes
- The Role of Risk Assessment in DD Treatment
- Identifying Harm Minimization Strategies
- Creating a Comprehensive Harm Minimization Plan
- Implementing and Monitoring the Plan: A Therapeutic Approach
Understanding Dissociative Disorder: Symptoms and Causes

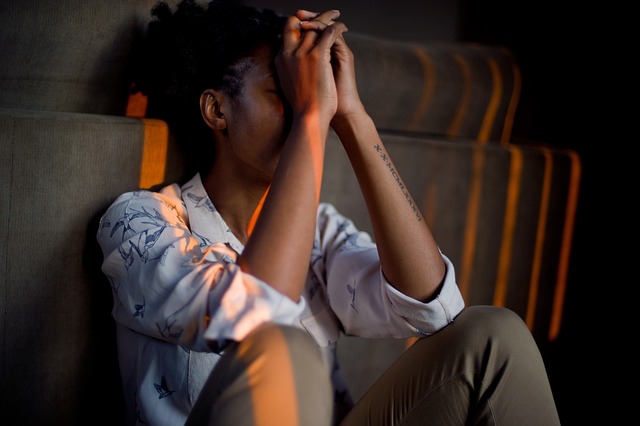
Dissociative Disorder is a complex mental health condition characterized by disruptions in an individual’s sense of identity and connection to their surroundings. This disorder often manifests as a coping mechanism in response to severe trauma or distressing life events. Symptoms can include episodes of amnesia, where individuals forget important personal information, alter egoes or distinct personalities, and a distorted sense of self. People with Dissociative Disorder may experience feelings of detachment from their bodies, leading to a sense of unreality. These symptoms can significantly impact daily functioning and relationships.
The causes are deeply rooted in traumatic experiences such as physical or emotional abuse, neglect, severe accidents, or prolonged exposure to life-threatening situations. Over time, the mind creates a dissociation mechanism to protect itself from overwhelming emotions and memories. However, without proper understanding and therapy for Dissociative Disorder, such as cognitive behavioral therapy or trauma-focused approaches, individuals may struggle with their symptoms. Effective treatment also involves learning conflict resolution techniques, compassion cultivation practices, and crisis intervention guidance to help manage and integrate diverse aspects of the self.
The Role of Risk Assessment in DD Treatment

Risk assessment plays a pivotal role in the therapy for Dissociative Disorder (DD), guiding treatment strategies and ensuring patient safety. It involves meticulously evaluating various aspects of a patient’s life, including their traumatic history, current symptoms, and potential triggers, to identify hazards that could exacerbate dissociation or lead to further harm. This process is crucial in developing a tailored harm minimization plan, which focuses on proactive measures to protect the individual during therapy.
By incorporating emotional intelligence and mental health awareness, therapists can facilitate effective emotional healing processes. Risk assessment enables them to tailor interventions aimed at regulating emotions, improving communication, and enhancing coping mechanisms. This holistic approach ensures that therapy for DD not only addresses symptoms but also empowers individuals with the skills to navigate their emotional landscapes safely and securely.
Identifying Harm Minimization Strategies

Identifying harm minimization strategies is a crucial step in risk assessment for mental health professionals, especially when addressing complex issues like Dissociative Disorder. Therapy for this condition often involves intricate and delicate processes, necessitating tailored approaches to ensure patient safety and well-being. One effective strategy is integrating comprehensive stress management techniques into treatment plans. By teaching patients coping mechanisms and mindfulness practices, healthcare providers can empower them to navigate stressful situations without triggering dissociative episodes.
Moreover, burnout prevention strategies for healthcare providers themselves are essential components of harm minimization. Mental health professionals dealing with high-risk cases may face significant emotional and physical strain. Implementing risk management planning involves setting clear boundaries, encouraging self-care practices, and fostering a supportive work environment. This not only reduces the risk of professional burnout but also enhances the overall quality of care provided to patients, including those suffering from Dissociative Disorder.
Creating a Comprehensive Harm Minimization Plan

A Comprehensive Harm Minimization Plan is an essential tool for addressing potential risks and mitigating harm, especially in cases involving complex mental health conditions such as Dissociative Disorder. This plan should be meticulously crafted, incorporating a multi-faceted approach to ensure the well-being of individuals affected. It begins with a thorough assessment of the individual’s history, triggers, and coping mechanisms. By understanding these factors, professionals can develop tailored strategies to prevent and manage crises.
The plan should encompass various elements, including Crisis Intervention Guidance to provide immediate support during acute episodes, Public Awareness Campaigns Development to educate communities about Dissociative Disorder and reduce stigma, and Depression Prevention measures as co-morbidities are common. Regular review and adaptation of the plan are crucial, as it allows for a dynamic response to evolving needs, ensuring long-term stability and improved quality of life.
Implementing and Monitoring the Plan: A Therapeutic Approach

Implementing a harm minimization plan is not just a one-time task but requires ongoing monitoring and adjustment. This process involves a therapeutic approach where individuals with dissociative disorders or similar conditions actively participate in managing their risks. Regular sessions with therapists can facilitate this, employing evidence-based practices like communication strategies and compassion cultivation techniques. These methods empower clients to identify triggers, develop coping mechanisms, and make informed decisions regarding their well-being.
The monitoring phase is crucial for evaluating the effectiveness of the harm minimization plan. Through regular review, therapists can assess changes in the client’s condition, adapt strategies as needed, and ensure compliance with mental health policy guidelines. This proactive approach fosters a supportive environment, encourages self-awareness, and promotes positive outcomes, ultimately enhancing the quality of life for individuals navigating dissociative disorders.
Risk assessment and harm minimization planning are essential components of therapy for Dissociative Disorder (DD). By understanding the symptoms, causes, and role of risk assessment in DD treatment, therapists can identify effective harm minimization strategies. Creating a comprehensive plan involves a collaborative approach with the client, considering individual needs and goals. Successful implementation and monitoring of this plan not only enhance safety but also foster healing and recovery for those living with DD.