Risk assessment is a critical process in therapy for children with chronic illnesses, focusing on physical and emotional risks. By identifying and addressing these, healthcare professionals can develop personalized harm minimization strategies to support each child's recovery and resilience. These strategies go beyond medical treatment, encompassing anxiety relief, social skills training, and communication tools, enabling children to manage their conditions effectively and improve their quality of life. This holistic approach, proven successful through case studies, leads to better outcomes and empowers kids to cope with chronic illnesses.
Risk assessment and harm minimization planning are essential components of providing safe and effective therapy for children with chronic illnesses. This comprehensive guide delves into the critical process of understanding risk assessment in pediatric chronic illness therapy, implementing targeted harm minimization strategies, and exploring successful case studies from healthcare settings worldwide. By learning from these approaches, professionals can enhance patient safety and outcomes.
- Understanding Risk Assessment in Pediatric Chronic Illness Therapy
- Implementing Harm Minimization Strategies for Young Patients
- Case Studies: Successful Risk Management in Pediatric Healthcare Settings
Understanding Risk Assessment in Pediatric Chronic Illness Therapy

Risk assessment is a critical component of providing therapy for children with chronic illnesses, ensuring their safety and well-being throughout the treatment process. It involves identifying potential risks associated with the illness itself, the treatment plan, and various environmental factors that could negatively impact the child’s health. By thoroughly evaluating these risks, healthcare professionals can implement harm minimization strategies tailored to each patient’s unique needs.
In the context of therapy for children with chronic illnesses, risk assessment goes beyond physical health considerations. It encompasses emotional and psychological aspects as well. For instance, the Mental Wellness Podcast Series Production highlights the importance of addressing mental health concerns that often accompany chronic conditions. Trauma Support Services and Emotional Intelligence interventions can play a pivotal role in mitigating risks related to anxiety, depression, and trauma, which are prevalent among pediatric patients facing long-term health challenges. This holistic approach ensures that children receive comprehensive care, fostering not just physical recovery but also emotional resilience.
Implementing Harm Minimization Strategies for Young Patients

Implementing harm minimization strategies for young patients with chronic illnesses is a critical aspect of healthcare that requires tailored approaches. Therapy for children with chronic conditions often focuses on more than just treating the physical symptoms; it aims to provide comprehensive support addressing emotional, behavioral, and social challenges. Techniques such as anxiety relief methods, social skills training, and communication strategies can empower young patients to manage their conditions effectively and enhance their overall well-being.
By integrating these strategies into treatment plans, healthcare providers can help children develop coping mechanisms to navigate the complexities of living with a chronic illness. This proactive approach not only minimizes potential harm but also fosters resilience, promoting a better quality of life for young individuals as they learn to advocate for themselves and manage their health in an age-appropriate manner.
Case Studies: Successful Risk Management in Pediatric Healthcare Settings

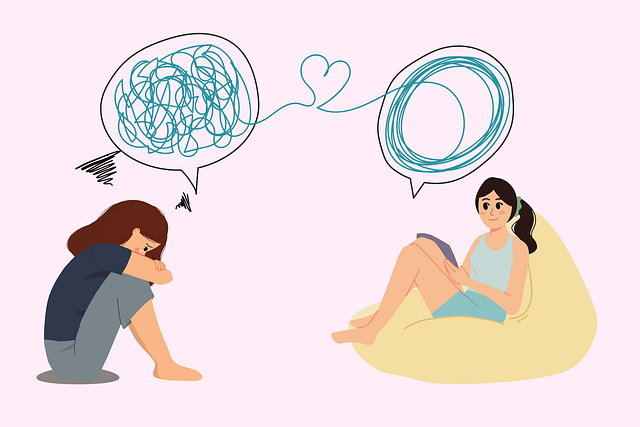
In pediatric healthcare settings, effective risk assessment and harm minimization planning have proven to be game-changers in ensuring safe and nurturing environments for young patients with chronic illnesses. Successful case studies highlight the power of tailored strategies that address not just physical health but also the psychological well-being of children. For instance, hospitals implementing mental illness stigma reduction efforts have seen improved patient outcomes, as children feel more comfortable seeking therapy for chronic conditions when they are supported in managing any associated anxiety or depression.
These initiatives often incorporate social skills training and communication strategies to foster a sense of belonging and reduce the impact of isolation. By integrating these approaches, healthcare providers not only enhance the effectiveness of treatments but also empower children to navigate their illnesses with enhanced coping mechanisms. This holistic view of care ensures that pediatric patients receive comprehensive support, ultimately improving their quality of life and promoting positive long-term health outcomes.
Risk assessment and harm minimization planning are indispensable tools in providing safe and effective therapy for children with chronic illnesses. By understanding the unique risks associated with pediatric care, healthcare professionals can implement tailored strategies to enhance patient outcomes. The case studies presented demonstrate that proactive risk management approaches not only minimize potential harms but also contribute to positive experiences for young patients, ensuring their well-being throughout their treatment journey.