Mental health policy is a multifaceted landscape that impacts access to quality care, such as Longmont Obsessive Compulsive Disorder (OCD) therapy. Stigma significantly hinders access and treatment, affecting policy design and funding. Advocacy must focus on mental health awareness through education and dispelling myths about OCD. In Longmont, Colorado, local initiatives promote specialized OCD therapy, including compassion cultivation practices and cognitive-behavioral therapy (CBT). Analyzing policies reveals weaknesses like insufficient funding and integrated service delivery, demanding targeted advocacy. Effective policy change leverages empathy, personal stories, data, and resilience-building for healthcare providers to improve service quality and outcomes.
Mental health policy advocacy is a powerful tool for creating positive change in communities. This article explores key aspects of mental health policy analysis, from understanding the foundation of advocacy to addressing the impact of stigma and unlocking access to care, such as the potential benefits of Longmont Obsessive Compulsive Disorder Therapy. We analyze existing policies, highlighting strengths, weaknesses, and gaps, and provide strategies for effective advocacy to ensure comprehensive and inclusive mental health support.
- Understanding Mental Health Policy: A Foundation for Advocacy
- The Impact of Stigma and Its Role in Shaping Public Policy
- Longmont Obsessive Compulsive Disorder Therapy: Unlocking Access to Care
- Analyzing Existing Policies: Strengths, Weaknesses, and Gaps
- Strategies for Effective Mental Health Policy Advocacy
Understanding Mental Health Policy: A Foundation for Advocacy

Mental health policy is a complex and multifaceted area that forms the backbone of advocacy efforts aimed at improving access to quality care. Understanding this policy landscape is crucial for anyone involved in mental health treatment, including professionals like those offering Longmont Obsessive Compulsive Disorder Therapy. By unraveling the intricacies of policy mechanisms, advocates can identify gaps and opportunities to drive positive change.
This involves recognizing the interplay between legislation, funding allocation, healthcare provider training (such as Burnout Prevention Strategies and Healthcare Provider Cultural Competency Training), and community support systems. Emotional Intelligence plays a significant role in navigating these policies, enabling advocates to communicate effectively with stakeholders and ensure that policy decisions reflect the diverse needs of individuals struggling with mental health issues.
The Impact of Stigma and Its Role in Shaping Public Policy

Stigma surrounding mental health issues remains a significant barrier to access and treatment, with profound implications for public policy. Often, individuals facing conditions like Longmont Obsessive Compulsive Disorder (OCD) therapy face societal and self-imposed isolation due to misunderstandings and fear of judgment. This stigma not only hinders people from seeking help but also shapes the way mental health services are designed and funded by governments. Public policies often reflect societal attitudes, and as such, they can either perpetuate or mitigate the effects of mental health stigma.
A crucial step in policy advocacy is thus to foster Mental Health Awareness through community outreach programs that educate the public and dispel myths surrounding conditions like OCD. By promoting understanding and empathy, these initiatives pave the way for more inclusive policies that prioritize Stress Reduction Methods as essential components of healthcare systems. Ultimately, a policy landscape free from stigma encourages early intervention, improves treatment outcomes, and ensures equitable access to mental health services for all.
Longmont Obsessive Compulsive Disorder Therapy: Unlocking Access to Care

In Longmont, Colorado, access to specialized therapy for Obsessive Compulsive Disorder (OCD) has been a growing focus in mental health advocacy. This small city has recognized the unique challenges faced by individuals dealing with OCD, a debilitating mental illness characterized by intrusive thoughts and repetitive behaviors. To address this, local initiatives have aimed to unlock care for those affected, ensuring that Longmont residents receive the necessary support.
One innovative approach is the integration of Compassion Cultivation Practices within therapy settings. By fostering understanding and reducing stigma associated with mental illness, these practices create a safe space for individuals struggling with OCD. In conjunction with traditional therapy methods, such as cognitive-behavioral therapy (CBT), this holistic strategy has shown promising results in managing symptoms and improving overall well-being. Longmont’s commitment to expanding Trauma Support Services further strengthens its mental health infrastructure, making it easier for those with OCD to access the specialized care they deserve.
Analyzing Existing Policies: Strengths, Weaknesses, and Gaps

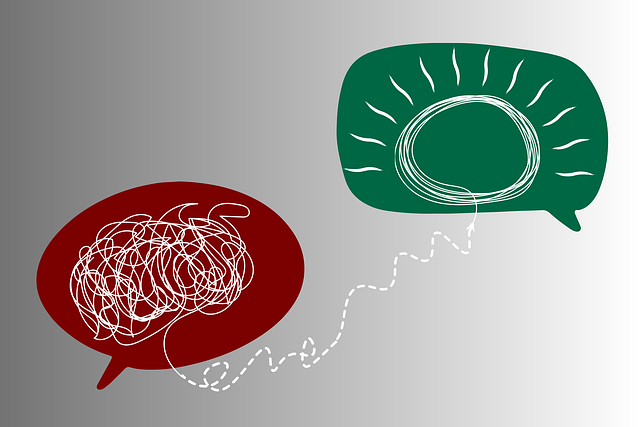
Analyzing existing mental health policies is a crucial step in advocating for better support systems. In any region, including those with renowned services like Longmont Obsessive Compulsive Disorder Therapy, there are inherent strengths and weaknesses within policy frameworks. The strengths often lie in well-intentioned legislation that promotes accessibility to healthcare provider cultural competency training, ensuring diverse professionals can offer specialized coping skills development and evidence-based practices such as mindfulness meditation for varied patient needs.
However, the weaknesses and gaps reveal critical areas of improvement. Policy loopholes may exist in terms of funding allocation, leading to disparities in access to quality care. There might also be a lack of integration between various services, hindering comprehensive mental health support. Identifying these shortcomings is essential to drive policy advocacy, pushing for more inclusive and effective strategies that cater to diverse communities’ needs.
Strategies for Effective Mental Health Policy Advocacy

Mental health policy advocacy requires a strategic approach to drive meaningful change. One effective method is to leverage empathy-building strategies, ensuring that policymakers understand the lived experiences of individuals with mental health conditions like Longmont Obsessive Compulsive Disorder (OCD) therapy patients. By sharing personal stories and utilizing data that highlights the impact of inadequate support systems, advocates can create a compelling narrative that fosters sympathy and drives policy action.
Additionally, resilience-building initiatives and burnout prevention strategies for healthcare providers should be integrated into mental health policy advocacy. This includes addressing workload issues, promoting work-life balance, and providing regular professional development opportunities. Such measures not only ensure the well-being of healthcare providers but also enhance the quality of mental health services delivered to patients, ultimately contributing to more effective policy outcomes.
Mental health policy advocacy is a multifaceted approach that requires understanding the intricate dynamics of public policy while addressing the profound impact of stigma. By analyzing existing policies, including unique initiatives like Longmont Obsessive Compulsive Disorder Therapy, we can identify strengths and weaknesses to advocate for more comprehensive and inclusive care. Effective advocacy strategies focus on removing barriers to treatment, reducing stigma, and ensuring equitable access to mental health services. These efforts are crucial in creating a healthier society where individuals with OCD, or any mental health condition, can lead fulfilling lives.