Diagnosing mental illness in young adults is hindered by stigma, lack of awareness, limited access to services, and cultural diversity. Cultural competency training for healthcare providers enhances diagnosis accuracy through improved sensitivity, encouraging tailored care and trust-building communication. Effective strategies include open dialogue, CBT, and educating on treatment benefits, addressing co-occurring disorders like depression, anxiety, and substance abuse. Enhancing diagnosis accuracy with advanced tools and early intervention leads to better patient outcomes, hope, and resilience in young adults seeking therapy, focusing on appropriate therapy for Young Adults.
Mental illness diagnosis accuracy is a critical area of focus, especially for young adults. This demographic faces unique challenges, with misdiagnosis rates alarmingly high, impacting treatment plans and patient outcomes significantly. The current state demands innovative solutions. By exploring advanced assessment tools, integrating technology like AI and digital therapy platforms, and implementing personalized therapy models, we can improve diagnosis accuracy and enhance the effectiveness of therapy for young adults.
- The Current State of Mental Illness Diagnosis for Young Adults
- – Exploring common challenges and misdiagnoses
- – Impact on treatment plans and patient outcomes
The Current State of Mental Illness Diagnosis for Young Adults

The process of diagnosing mental illness in young adults is a complex and often challenging endeavor. Despite advancements in healthcare, the current state of diagnosis reveals several areas for improvement, especially within this demographic. Many young adults face barriers to accessing accurate assessments due to various factors, including stigma, lack of awareness, and limited access to specialized services. This age group tends to present unique symptoms and experiences that can be easily overlooked or misinterpreted, leading to delays in treatment. For instance, emotional intelligence and communication strategies often play a crucial role in how young adults express their struggles, which may differ from traditional presentation patterns.
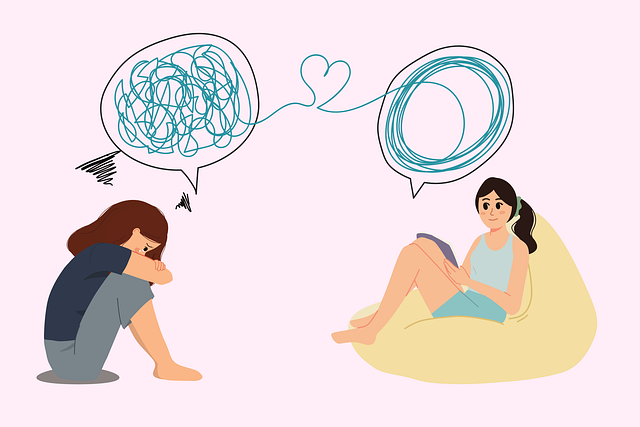
The impact of cultural competency training for healthcare providers cannot be overstated. With the diverse nature of young adult populations, understanding cultural nuances is essential. Training that enhances cultural sensitivity and knowledge ensures that mental health professionals can provide tailored care. By integrating these approaches, diagnosis accuracy may improve, leading to more effective therapy for young adults. Effective communication, when combined with a comprehensive assessment, can foster an environment where young adults feel heard, enabling them to seek the help they need without delay.
– Exploring common challenges and misdiagnoses

Mental health professionals often face a complex task when diagnosing young adults, as this age group presents with unique challenges and a wide range of potential conditions. One significant issue is the prevalence of co-occurring disorders, where individuals may struggle with depression, anxiety, or substance abuse in addition to other mental illnesses. This complexity can lead to misdiagnosis, especially when symptoms overlap between conditions. For instance, the energetic and impulsive nature often associated with borderline personality disorder (BPD) can be mistaken for attention-deficit/hyperactivity disorder (ADHD), which requires distinct treatment approaches.
Furthermore, young adults may resist traditional therapy methods, posing another challenge. This resistance could stem from various factors, such as a desire for independence, fear of judgment, or a lack of understanding about mental health. Effective communication strategies and emotional well-being promotion techniques are essential to engage this demographic. Encouraging open dialogue, educating on the benefits of treatment, and incorporating therapeutic methods tailored to their needs, like cognitive-behavioral therapy (CBT), can improve diagnosis accuracy and facilitate successful recovery journeys for young adults seeking therapy.
– Impact on treatment plans and patient outcomes

Mental illness diagnosis accuracy plays a pivotal role in shaping treatment plans and patient outcomes, especially when targeting young adults who often face unique challenges. Inaccurate diagnoses can lead to inappropriate or delayed therapy for Young Adults, which, in turn, exacerbates existing symptoms and may contribute to comorbid conditions such as anxiety relief and depression prevention becoming more entrenched. For instance, a misdiagnosed anxiety disorder might be treated with ineffective methods designed for depression, hindering the patient’s progress and overall well-being.
Efforts to enhance diagnosis accuracy are, therefore, essential for improving mental health care. These include refining assessment tools, integrating advanced risk assessment for mental health professionals, and promoting early intervention strategies. By ensuring precise diagnoses, healthcare providers can tailor therapy for young adults more effectively, addressing specific conditions with evidence-based approaches. This not only improves patient outcomes but also fosters a sense of hope and resilience among individuals navigating the complexities of their mental health journeys.
Mental illness diagnosis accuracy is a vital aspect of providing effective therapy for young adults. By understanding the current challenges, including misdiagnoses stemming from complex symptoms and individual variations, we can significantly improve patient outcomes. Enhanced training, evidence-based practices, and a shift towards personalized care are key strategies to ensure accurate diagnoses and successful treatment plans tailored to each young adult’s unique needs.