The current mental illness diagnosis system struggles with complexity and range, leading to misdiagnosis or delays, especially for gender identity issues. Arvada Gender Identity Therapy offers a nuanced approach, integrating self-care, compassion cultivation, and burnout prevention strategies to enhance diagnostic accuracy. This, coupled with ongoing research and education, aims to transform the process into a more effective, compassionate system, addressing societal biases and limited clinical training, particularly for marginalized communities.
Mental illness diagnosis accuracy remains a pressing challenge, with misdiagnoses and under-recognition prevalent despite advances in understanding. This article explores current hurdles, including societal biases and lack of diverse clinical training, hindering precise identification of mental health conditions. We present innovative strategies to enhance accuracy, such as the personalized approach of Arvada Gender Identity Therapy and the integration of AI tools in assessment. Additionally, we emphasize the crucial roles of education, advocacy, and collaboration for promoting diagnostic excellence.
- Current Challenges in Mental Illness Diagnosis
- – Discussion on common misdiagnoses and under-recognition of specific disorders
- – Impact of societal biases and lack of diverse clinical training on diagnosis accuracy
Current Challenges in Mental Illness Diagnosis

The current landscape of mental illness diagnosis is fraught with challenges that impact accuracy and patient care. One significant hurdle is the complex nature of human emotions and behaviors, which often manifest in diverse ways across different individuals and cultures. This complexity is further complicated by the vast array of mental health conditions, each with its unique set of symptoms, contributing factors, and treatment requirements. As a result, misdiagnosis or delayed diagnosis are not uncommon, leading to frustration for both patients and healthcare providers alike.
In the case of Arvada Gender Identity Therapy, addressing these challenges requires a nuanced approach that considers individual experiences and identities. The integration of self-care practices and compassion cultivation can enhance therapeutic outcomes. By promoting burnout prevention strategies among mental health professionals, we can ensure sustained empathy and attention to detail, thereby improving diagnosis accuracy. These efforts, combined with ongoing research and education, hold the key to transforming mental illness diagnosis into a more effective and compassionate process.
– Discussion on common misdiagnoses and under-recognition of specific disorders

Mental health professionals often face challenges in accurately diagnosing specific disorders, leading to misdiagnoses and under-recognition. This is particularly true for conditions on the spectrum of gender identity issues, such as those addressed by Arvada Gender Identity Therapy. For example, individuals experiencing gender dysphoria may be incorrectly labeled with other mental health conditions, like depression or anxiety, without a thorough exploration of their unique struggles related to gender congruence. Similarly, lesser-known disorders often fall through the cracks, resulting in delayed treatment and unnecessary suffering.
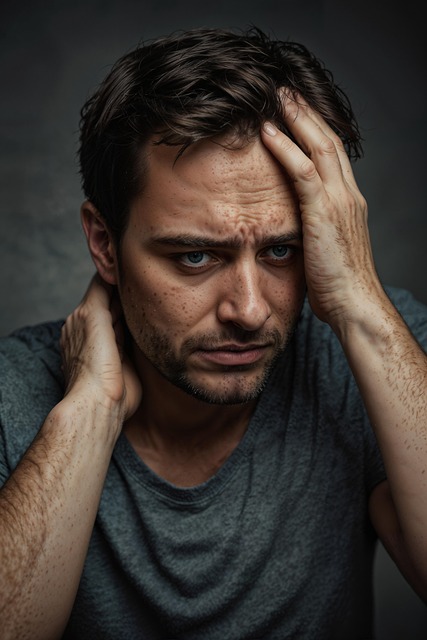
The impact of misdiagnosis is profound, affecting not only individuals’ access to appropriate care but also their emotional healing processes. It’s not uncommon for patients to experience a exacerbation of symptoms or feel disheartened when they encounter a diagnosis that doesn’t resonate with their lived experiences. To mitigate these issues, healthcare providers can benefit from enhanced training in crisis intervention guidance and burnout prevention strategies. Such initiatives would enable them to navigate complex cases more effectively and foster an environment where accurate diagnoses are prioritized, ultimately improving patient outcomes and the overall mental health landscape.
– Impact of societal biases and lack of diverse clinical training on diagnosis accuracy

Societal biases and a lack of diverse clinical training significantly impact the accuracy of mental illness diagnoses. Many healthcare professionals are trained primarily within a narrow set of cultural norms, often neglecting to account for the vast spectrum of human experiences and identities. This can lead to misdiagnoses or delayed recognition of conditions, especially among individuals from marginalized communities. For instance, Arvada Gender Identity Therapy has highlighted how gender dysphoria symptoms may be misunderstood or dismissed due to societal biases, affecting the quality of care received by transgender individuals.
Similarly, cultural differences in expressions of distress can create barriers. What might be considered normal behavior within one cultural context could signal a mental health issue in another. Effective diagnosis requires clinical trainers to expose future therapists to varied experiences through diverse case studies and interactive learning environments. Fostering an inclusive training environment that encourages the development of self-care routines for better mental health, along with communication strategies and anxiety relief techniques, can ultimately enhance diagnostic accuracy.
Mental illness diagnosis accuracy has been a long-standing challenge, exacerbated by societal biases and a lack of diverse clinical training. By acknowledging these issues, professionals can strive for improvement through enhanced education and inclusive practices. Initiatives like Arvada Gender Identity Therapy play a crucial role in fostering understanding and precision, ensuring individuals receive the appropriate care for their unique mental health needs. Continuous efforts to refine diagnosis methods are essential for better patient outcomes and a more supportive societal landscape.